TAFRO in Disguise: Idiopathic Multicentric Castleman Disease-Like Syndrome With Renal Thrombotic Microangiopathy and Autoimmune Overlap
DOI:
https://doi.org/10.14740/wjnu1006Keywords:
TAFRO syndrome, Idiopathic multicentric Castleman disease, Thrombocytopenia, Acute renal failure, Thrombotic microangiopathy, Reticulin fibrosis of bone marrow, Anti-IL-1 therapy, Anakinra, Anti-IL-6 therapy, Tocilizumab, Siltuximab, CyclosporineAbstract
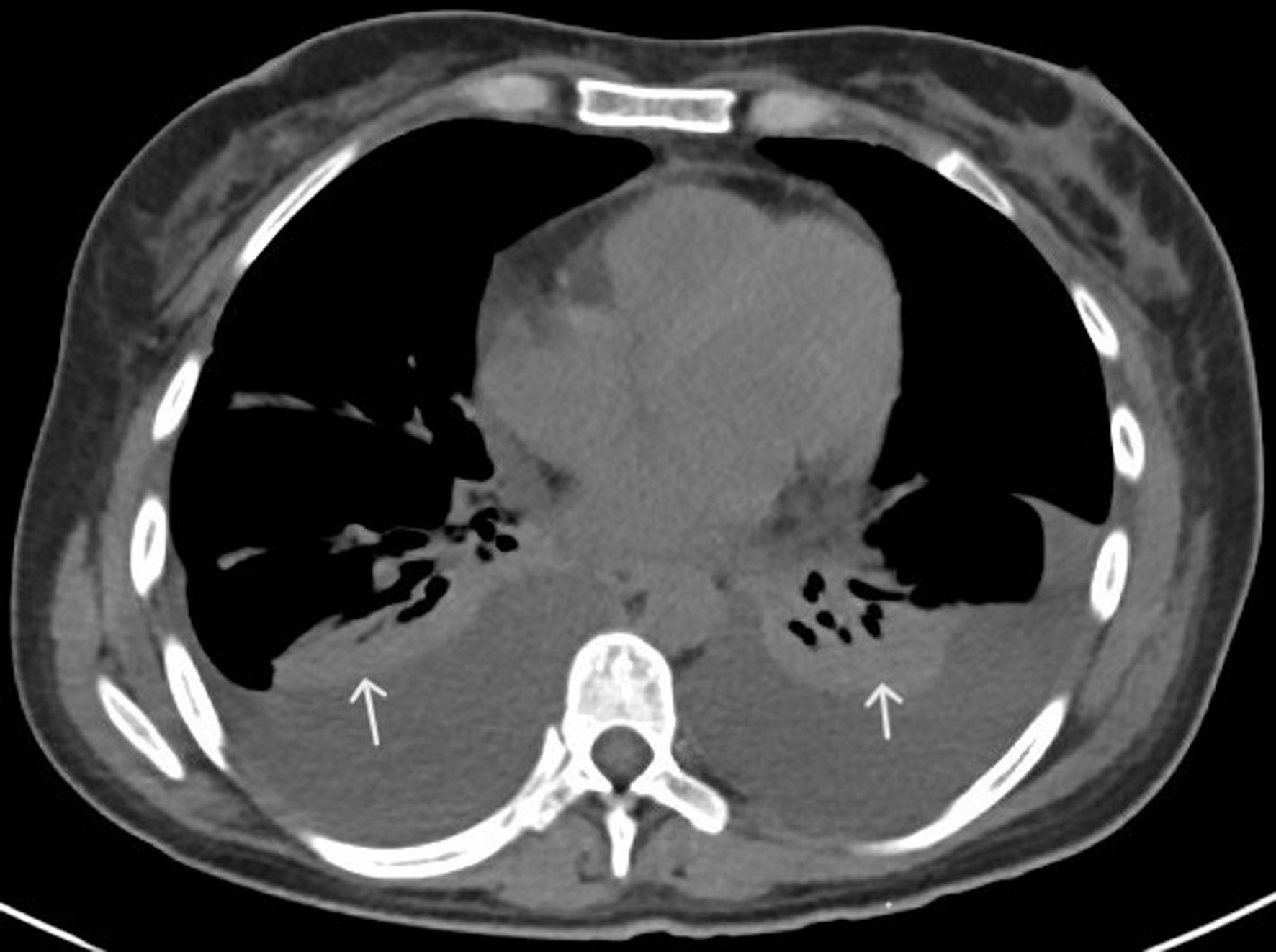
TAFRO syndrome is a rare systemic inflammatory disorder characterized by thrombocytopenia, anasarca, fever/elevated C-reactive protein (CRP), reticulin fibrosis of bone marrow/renal dysfunction, and organomegaly. It is considered an aggressive subtype of idiopathic multicentric Castleman disease (iMCD), typically requiring lymph node (LN) histopathology for definitive diagnosis. The cases lacking LN biopsy due to accessibility or severe systemic illness but meeting all the criteria for iMCD and TAFRO are categorized as TAFRO with possible iMCD. Another category well recognized in the literature is TAFRO associated with autoimmune diseases, especially Sjogren’s syndrome. We present a 29-year-old female patient with a history of seropositive rheumatoid arthritis, Sjogren’s syndrome, and Barrett’s esophagus who developed an abrupt onset of severe thrombocytopenia, anemia, generalized anasarca, high CRP levels, and renal dysfunction 3 weeks after a viral illness with gastrointestinal symptoms. Imaging revealed hepatosplenomegaly, retroperitoneal lymphadenopathy, and pleural effusion and ascites requiring drainage. Further analysis revealed hypoalbuminemia, elevated soluble interleukin-2 receptor (sIL-2R) and interleukin-6 (IL-6) levels, as well as negative human herpesvirus-8 (HHV-8), cytomegalovirus (CMV), and Epstein-Barr virus (EBV) serologies. ADAM metallopeptidase with thrombospondin type 1 motif 13 (ADAMST13) and complement studies were also negative. A bone marrow biopsy showed evidence of reticulin fibrosis, but an LN biopsy was not feasible. A renal biopsy demonstrated histopathological features consistent with thrombotic microangiopathy (TMA), a finding increasingly recognized in TAFRO. Additionally, elevated anti-Sjogren’s syndrome-related antigen A (SSA) antibodies were found, suggesting a possible autoimmune overlap. Given no LN biopsy, a diagnosis of “TAFRO syndrome with possible iMCD” with autoimmune overlap was entertained. The patient responded well to systemic corticosteroids, plasmapheresis, and anti-interleukin-1 (IL-1) therapy, anakinra. She was discharged in stable condition with improved clinical condition and renal function. The regimen was changed to anti-IL-6 therapy, sarilumab, in the immediate post-discharge period. This case is unique as it fulfills all six criteria of TAFRO syndrome and emphasizes the importance of recognizing it without an LN biopsy, TAFRO syndrome with possible iMCD, particularly when clinical, laboratory, and bone marrow findings support the diagnosis. This case further highlights the diagnostic complexity of TAFRO syndrome and the co-occurrence of renal TMA and autoimmune overlap, suggesting a potential interplay between multiple autoimmune cytokine-driven inflammatory processes. Prompt diagnosis and early immunosuppressive therapy are critical to improve systemic and renal outcomes in such cases with diagnostically ambiguous presentations.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.