| World Journal of Nephrology and Urology, ISSN 1927-1239 print, 1927-1247 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Nephrol Urol and Elmer Press Inc |
| Journal website https://wjnu.elmerpub.com |
Case Report
Volume 15, Number 1, January 2026, pages 13-17
Villous Adenoma of Ureteral Stump: An Unusual Presentation of Ureteral Stump Syndrome
Haleema Sadiaa, Aniqa Saeedb, Alka Ranic, Imran Khan Jalbanib, d
aAga Khan University, Stadium Road, PO Box 3500, Karachi 74800, Pakistan
bDepartment of Surgery, Aga Khan University, Stadium Road, PO Box 3500, Karachi 74800, Pakistan
cDepartment of Pathology and Laboratory Medicine, Aga Khan University, Stadium Road, PO Box 3500, Karachi 74800, Pakistan
dCorresponding Author: Imran Khan Jalbani, Department of Surgery, Aga Khan University, Karachi 74800, Pakistan
Manuscript submitted September 15, 2025, accepted December 27, 2025, published online January 10, 2026
Short title: Villous Adenoma of Ureteral Stump
doi: https://doi.org/10.14740/wjnu1015
| Abstract | ▴Top |
Ureteral stump syndrome (USS) is a rare condition occurring after nephrectomy due to residual ureteral pathology, including reflux, infection, calculi, empyema, or malignancy. A long ureteral stump may predispose patients to USS by promoting urine stasis. Ureterocutaneous fistula, a rare complication, requires accurate diagnosis to avoid unnecessary treatment. Management involves identification of cause and corrective measures including surgical excision. Malignant transformation, though rare, underscores the need for thorough pre-treatment assessment. A multidisciplinary approach integrating clinical, radiological, and microbiological evidence is essential for effective diagnosis. We hereby present a first case of villous adenoma of ureteral stump.
Keywords: Ureteral stump syndrome; Villous adenoma; Ureterocutaneous fistula; Nephrectomy; Rare urological tumor
| Introduction | ▴Top |
Nephrectomy remains the standard treatment for symptomatic non-functioning kidney, although the complete resection of the ipsilateral ureter remains a subject of debate. While complete ureteral removal is rarely indicated, it may help prevent the development of ureteral stump syndrome (USS), which occurs when a portion of the ureter referred to as the ureteral stump is left behind following nephrectomy [1]. USS is a rare complication, with an incidence of approximately 0.8-1%, and can present with a wide range of symptoms, including febrile urinary tract infections, hematuria, flank pain, abscess formation, stones, empyema, strictures, and even malignancies [1-3]. Additionally, fistula formation, such as ureterocutaneous and ureterouterine fistulas, has also been reported following nephrectomy [3, 4].
We present a case of ureterocutaneous fistula formation with villous adenoma of ureteral stump occurring 25 years after a simple nephrectomy, complicated by enterocutaneous fistula formation and recurrent episodes of abscess formation in the intervening years.
| Case Report | ▴Top |
Investigations
A female patient in her mid-30s was referred to our department with a 4-month history of swelling, purulent discharge, and pain in the left flank region. Her past medical history was significant for a left-sided nephrectomy as a teenager, performed for a non-functioning kidney secondary to multiple renal calculi and chronic pyelonephritis. In the years that followed, she experienced recurrent fever and left flank pain despite completing multiple courses of antibiotics and a 6-month course of antitubercular therapy (ATT), administered empirically in a tuberculosis (TB) endemic region [5]. This ultimately led to an incision and drainage procedure at the nephrectomy site.
The persistence of symptoms led to an exploratory laparotomy, which yielded insignificant findings. This was followed by a second empiric course of ATT. Subsequently, the patient developed serous discharge from the left iliac region. Imaging revealed soft tissue thickening and calcification in the left psoas, consistent with an abscess, prompting a third empiric course of ATT; however, she never tested positive for TB. Despite ongoing medical and surgical interventions, the patient continued to experience persistent left flank pain and recurrent fevers, leading to another exploratory laparotomy within the same year. This revealed an enterocutaneous fistula, necessitating a colon resection and a Hartmann’s procedure, which was reversed 4 months later. In the ensuing years, the patient experienced recurrent urinary tract infections caused by Escherichia coli (E. coli), which responded well to appropriate antibiotic therapy.
As shown in Figure 1, prior to presenting to our clinic, the patient underwent drainage of a left flank abscess, during which thick, gelatinous pus-like material was drained. However, this did not lead to resolution of symptoms. The patient subsequently presented with complaints of left flank pain, swelling, and purulent discharge without any odor, which worsened during urination. These symptoms were accompanied by burning micturition and lower urinary tract symptoms, including straining, intermittency, and hesitancy.
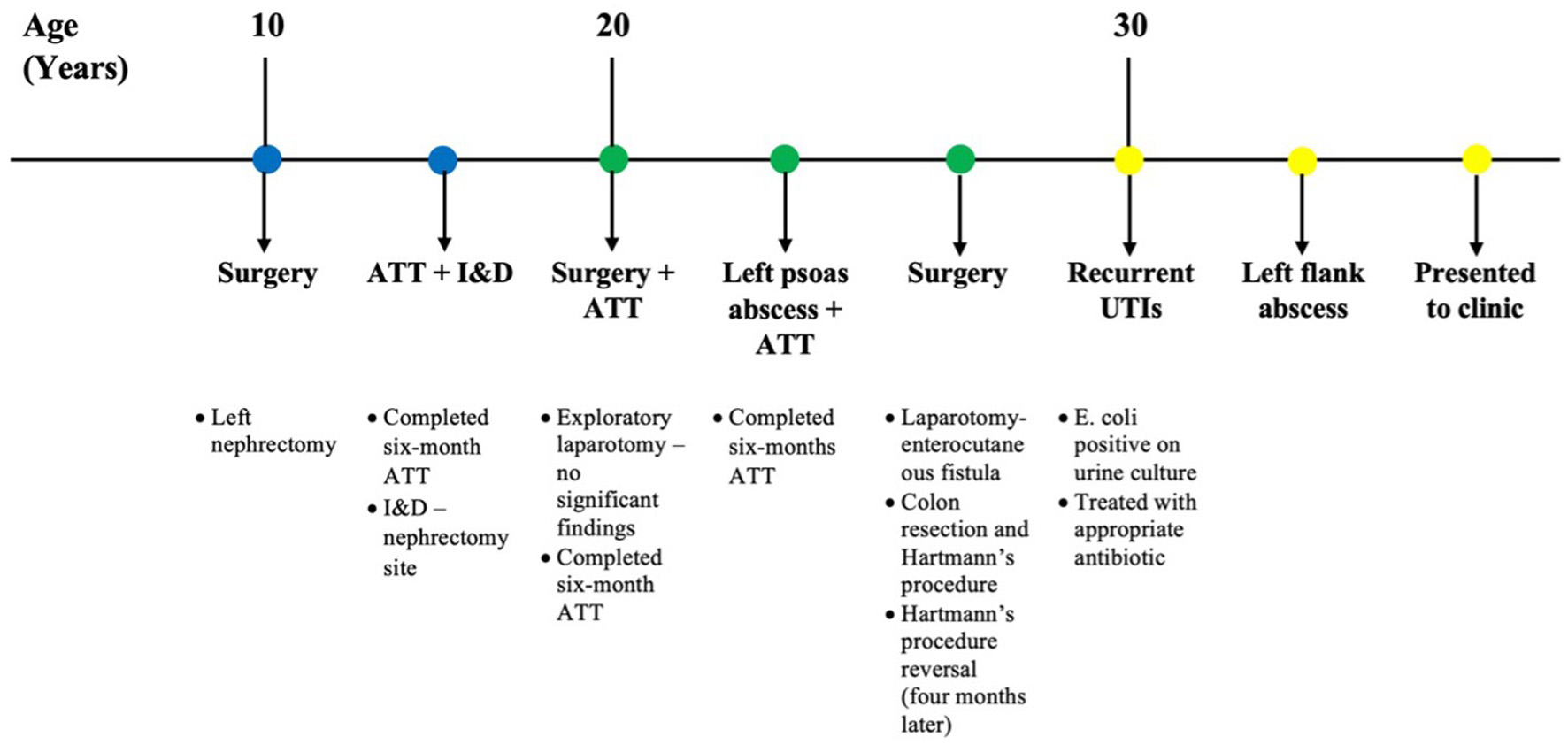 Click for large image | Figure 1. Clinical timeline of the patient’s course prior to presentation at our clinic, highlighting major interventions and symptom progression. ATT: antitubercular therapy; E. coli: Escherichia coli; I&D: incision and drainage; UTI: urinary tract infection. |
The physical exam revealed multiple healed surgical scars arranged in a haphazard manner. A small tract was identified in the left flank area, which revealed a scant amount of purulent discharge, with no surrounding erythema or warmth. No increased drainage was observed with the Valsalva maneuver.
The cytology of the thick, gelatinous pus drained from the left flank prior to presentation at our clinic revealed proteinaceous material with inflammatory cells, and cultures were positive for E. coli, although the interferon gamma release assay for tuberculosis (IGRA TB) test was negative.
A contrast-enhanced computed tomography (CT) scan (Fig. 2) was ordered, which revealed a large cutaneous fistula in the lumbar region extending to the urinary bladder, with potential involvement of the left distal ureter, although no contrast reflux was observed within the fistula tract. The fistula tract measured approximately 28 mm to the skin surface.
 Click for large image | Figure 2. Transverse plane of contrast-enhanced computed tomography (CT) scan showing a cutaneous tract on the left side measuring approximately 28 mm in length (arrow), along with evidence of prior left nephrectomy. |
Diagnosis
The patient’s long-standing history of chronic left flank pain, recurrent fevers, and prior surgeries raised several differential diagnoses. The multiple surgeries, along with completed courses of ATT in a TB-endemic region, raised concerns for tubercular involvement of the genitourinary tract, potentially manifesting as a ureteric stricture or fistula. However, the lack of improvement after multiple courses of ATT, a negative IGRA, and the presence of a cutaneous fistula on CT imaging raised suspicion for a ureterocutaneous fistula as a complication of the ureteral stump following nephrectomy.
Treatment
The patient underwent a distal ureterectomy with excision of the bladder cuff and sinus tract. Initial flexible cystoscopy revealed a dilated ureter filled with gelatinous material. The surgical approach was made through an extended modified Rutherford-Morrison incision in the left iliac fossa. Intraoperatively, due to dense adhesions and the colon being attached to the distal ureter, dissection proved challenging. Approximately 15 cm of the ureter (Fig. 3) was excised, extending from the bladder to the skin, and the bladder was closed at the ureteral orifice.
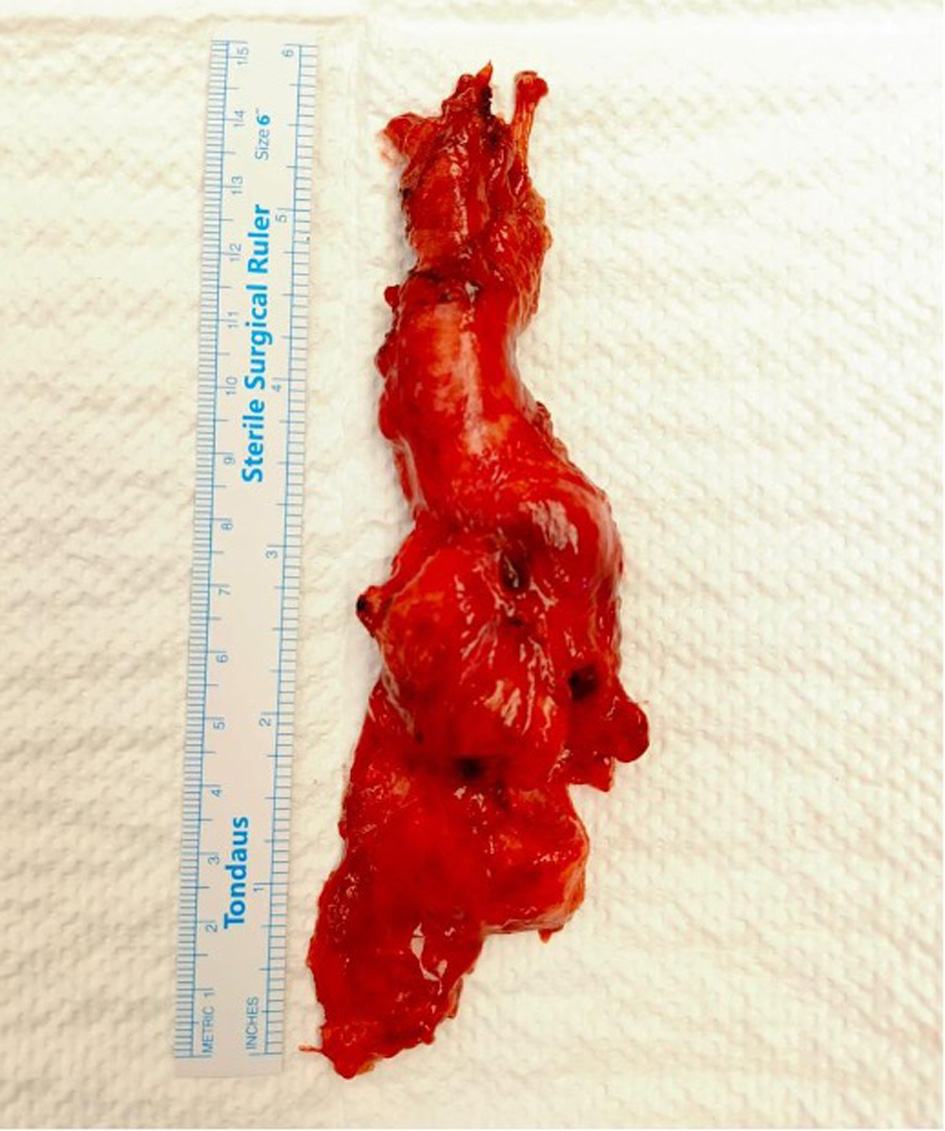 Click for large image | Figure 3. Gross specimen of the excised left ureter measuring approximately 15 cm. |
Follow-up and outcomes
Postoperatively, the patient had an uneventful recovery. The drain and catheter were removed on the second postoperative day. The sinus tract was managed with daily dressings until it healed by secondary intention. Histopathology revealed villous adenoma of the ureter, with no evidence of high-grade dysplasia or malignancy. Similarly, histopathology of the ureteral stump confirmed villous adenoma without signs of high-grade dysplasia or malignancy. As shown in Figure 4, there were no high-grade nuclear features or significant mitotic activity, confirming the benign nature of the disease. The patient was followed up in the clinic after discharge and had no complaints or complications.
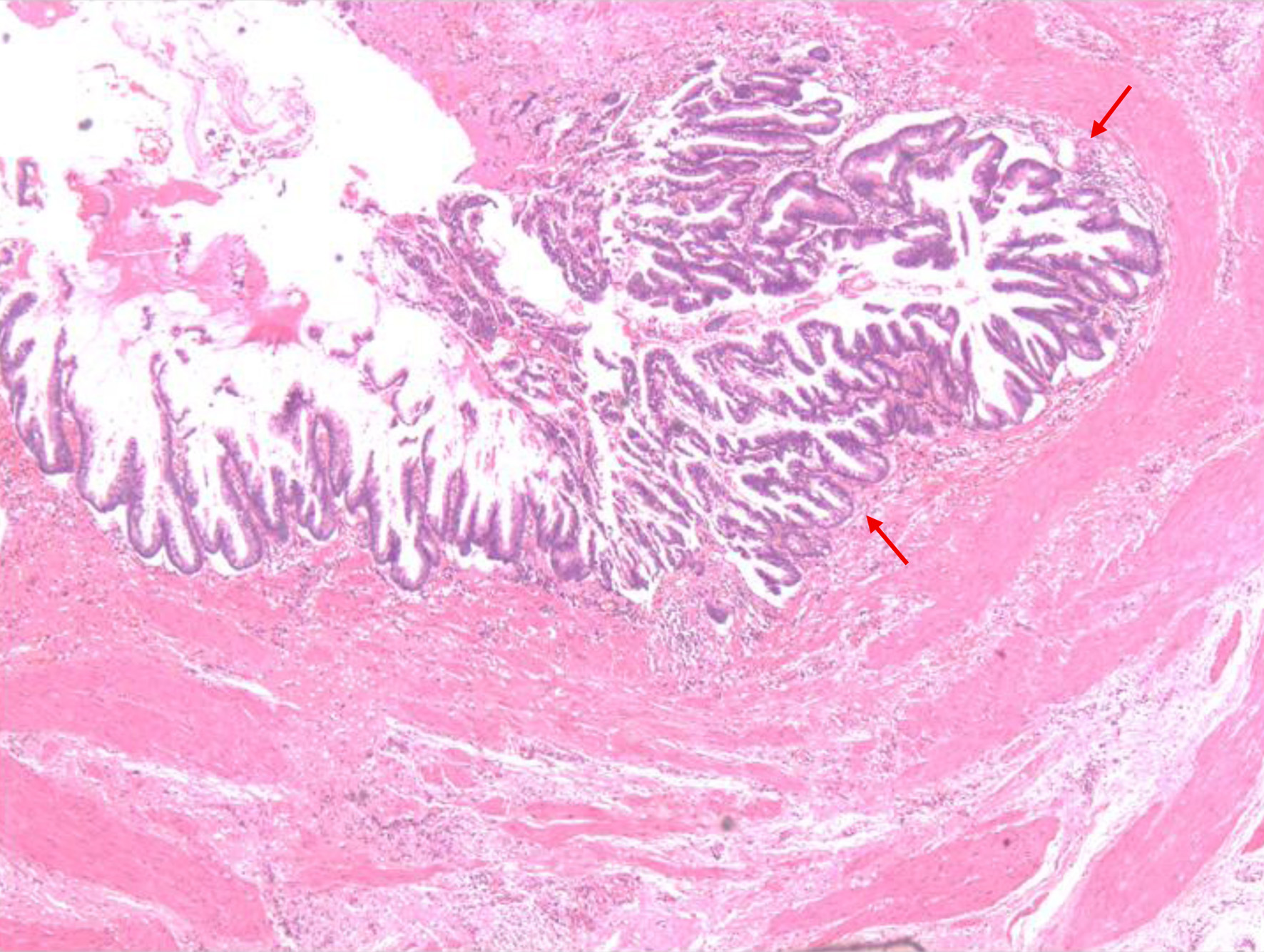 Click for large image | Figure 4. Histopathological section of the ureteric wall showing a lesion with papillary configuration, composed of fused tubules lined by columnar epithelium and goblet cells exhibiting pseudostratification and low-grade dysplasia (arrows). No evidence of muscularis or vascular invasion is identified. |
| Discussion | ▴Top |
USS occurs when the remaining segment of the ureter, left in place after a nephrectomy, becomes symptomatic. This condition is often overlooked, as its symptoms are commonly attributed to non-urological causes. However, it typically arises due to underlying pathological processes such as reflux, infection, calculi formation, empyema, and malignancy [1]. The pathogenesis of USS following nephrectomy is not fully understood, though one theory suggests that a long ureteral stump may function like a bladder diverticulum, increasing the risk of USS. In contrast, shorter ureteral stumps are less prone to USS as they effectively drain urine due to retained peristaltic activity [6]. Another theory suggest that well-draining ureters may undergo atrophy over time, but the presence of reflux potentially caused by neurovascular damage during the initial surgery along with voiding dysfunction, obstructions like stones, or foreign bodies, can contribute to the development of USS [7].
A ureterocutaneous fistula, characterized by an abnormal tract between the ureter and the skin, is a rare manifestation of USS post-nephrectomy. It typically presents persistent discharge from the fistula site, which may be further complicated by secondary infections or even sepsis. In cases of suspected fistula, sinus drainage, or abscess formation, it is essential to rule out genitourinary TB through swab or pus culture and sensitivity tests, along with a contrast-enhanced CT scan to detect any associated collections [8]. In regions where TB is endemic, inconclusive diagnostic results often lead to unnecessary treatment with ATT. This was evident in our patient’s case, as she never tested positive for any TB diagnostic test yet underwent three full courses of ATT. Such instances highlight the critical need for accurate diagnosis and careful clinical judgment, particularly in cases where the diagnosis remains uncertain. Failure to do so not only results in over-treatment, exposing patients to potential drug toxicity and unnecessary psychological and financial burden, but also increases the risk of under-treatment in cases where the true underlying condition remains undiagnosed. A balanced approach, combining clinical, radiological, and microbiological evidence, is essential to ensure appropriate management and prevent both overt treatment and unnecessary interventions [9].
The optimal treatment for retained ureter is simple excision, performed either via open or laparoscopic procedure. However, endourological techniques are emerging as feasible management alternatives for USS [10]. In complicated cases presenting with ureterocutaneous fistula, management is mainly based on complete excision of tract. In our case, endourological or laparoscopic approach was not possible due to multiple surgical intervention. The primary reason for performing retrograde ureterography or directly visualizing the ureteral stump before proceeding with the chosen treatment approach is to rule out the rare but clinically significant risk of ureteral stump cancer. Although uncommon, malignant transformation within the residual ureter can occur and may go undetected without thorough evaluation [11].
A study by Kim et al [12] highlighted this concern, reporting eight cases of ureteral stump cancer among 318 patients who had undergone nephrectomy for benign conditions. Of these, six were diagnosed with transitional cell carcinoma, while two had squamous cell carcinoma. These findings underscore the importance of pre-treatment assessment to ensure early detection and appropriate management, thereby preventing delayed diagnosis and associated complications. No case of villous adenoma of USS has ever been reported in literature. Villous adenomas of the urinary tract are rare, being most common in the urinary bladder, followed by the urethra. Morphological features of these tumors are like those of the colonic adenomas [12].
Villous adenomas of the urinary tract are rare glandular lesions that display colonic-type, villoglandular architecture and intestinal metaplasia. They usually have varied CK7 expression and are CK20 and carcinoembryonic antigen (CEA) positive, indicating intestinal differentiation rather than urothelial lineage. Although villous adenomas are typically benign and can be successfully treated with complete excision, their known association with adenocarcinoma makes them clinically significant. Case series and reviews report coexisting adenocarcinoma in few cases (roughly one-third in some series), which necessitates careful histologic examination and extensive sampling to rule out invasion [13, 14]. Therefore, both histologically (intestinal-type villous architecture versus glandular or urothelial malignant histology) and biologically (usually non-invasive when pure), our lesion differs from stump adenocarcinoma or urothelial carcinoma. However, monitoring for synchronous or metachronous malignant transformation is still crucial and warrants thorough excision and careful monitoring.
Learning points
The diagnosis of USS is difficult due to its varied clinical presentations. Radiological investigations are crucial in detecting USS and guiding management decisions. Completion ureterectomy remains the definitive treatment, whether performed through an open or laparoscopic approach. Contemporary literature does not universally support complete ureterectomy in all cases following simple nephrectomy. This case highlights the importance of remaining vigilant to varied presentation, ensuring prompt diagnosis, and providing appropriate management.
Acknowledgments
None to declare.
Financial Disclosure
The authors declare no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Written informed consent was taken from the patient for the publication of this case report and accompanying images.
Author Contributions
Haleema Sadia: writing – project administration, original draft, and writing – review and editing. Aneeqa Saeed: data curation, writing – original draft, and writing – review and editing. Alka Rani: investigation and writing – review and editing. Imran Khan Jalbani: conceptualization, guarantor, supervision, and writing – review and editing. All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Labanaris AP, Zugor V, Smiszek R, Nutzel R, Kuhn R. Empyema of the ureteral stump. An unusual complication following nephrectomy. ScientificWorldJournal. 2010;10:380-383.
doi pubmed - Arora S, Yadav P, Ansari MS. Diagnosis and management of symptomatic residual ureteral stump after nephrectomy. BMJ Case Rep. 2015;2015:bcr2015209441.
doi pubmed - L DCDMMC. Case report: symptomatic ureteral stump after nephrectomy. AUA News. 2023.
- Yalcin MYI; Karabicak M, Ergani B, Cetin T, Ozbilen MH, Suelozgen T, Koc G, et al. Nephrocutaneous fistula: An unusual nephrectomy indication in percutaneous nephrolithotomy. Journal of Urological Surgery. 2019;6(1):59-61.
- Kumar R. Empirical use of antituberculosis drugs should not be equated to their inappropriate and indiscriminate use. Indian J Pharmacol. 2011;43(3):363-364.
doi pubmed - Androulakakis PA, Stephanidis A, Antoniou A, Christophoridis C. Outcome of the distal ureteric stump after (hemi)nephrectomy and subtotal ureterectomy for reflux or obstruction. BJU Int. 2001;88(6):586-589.
doi pubmed - Iaquinto M, Esposito C, Escolino M, Farina A, Settimi A, Cigliano B. Symptomatic refluxing distal ureteral stump after retroperitoneoscopic nephrectomy. APSP J Case Rep. 2014;5(1):14.
pubmed - Kacem A, Raboudi M, Mansouri N, Gargouri F, Dridi M, Ghozzi S. A rare case of ureteral tuberculosis mimicking a tumor. Urol Case Rep. 2022;44:102147.
doi pubmed - Krishnamoorthy S, Palaniyandi V, Kumaresan N, Govindaraju S, Rajasekaran J, Murugappan I, Ramanan V, et al. Aspects of evolving genito urinary tuberculosis-a profile of genito urinary tuberculosis (GUTB) in 110 patients. J Clin Diagn Res. 2017;11(9):PC01-PC05.
doi pubmed - De Caluwe D, Chertin B, Puri P. Fate of the retained ureteral stump after upper pole heminephrectomy in duplex kidneys. J Urol. 2002;168(2):679-680.
doi pubmed - Biswas K, Singh AG, Ganpule AP, Sabnis RB, Desai MR. Clinical features and management of ureteric stump syndrome: Single-centre experience and contemporary literature review. Asian J Urol. 2022;9(2):193-196.
doi pubmed - Kim YJ, Jeon SH, Huh JS, Chang SG. Long-term follow-up of ureteral stump tumors after nephrectomy for benign renal disease. Eur Urol. 2004;46(6):748-752.
doi pubmed - Cheng L, Montironi R, Bostwick DG. Villous adenoma of the urinary tract: a report of 23 cases, including 8 with coexistent adenocarcinoma. Am J Surg Pathol. 1999;23(7):764-771.
doi pubmed - Seibel JL, Prasad S, Weiss RE, Bancila E, Epstein JI. Villous adenoma of the urinary tract: a lesion frequently associated with malignancy. Hum Pathol. 2002;33(2):236-241.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY 4.0), which permits unrestricted use, distribution, and reproduction in any medium, including commercial use, provided the original work is properly cited.
World Journal of Nephrology and Urology is published by Elmer Press Inc.