| World Journal of Nephrology and Urology, ISSN 1927-1239 print, 1927-1247 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Nephrol Urol and Elmer Press Inc |
| Journal website https://www.wjnu.org |
Case Report
Volume 000, Number 000, December 2024, pages 000-000
Leiomyoma Associated With Epithelial Dysplasia of the Urinary Bladder: Cytopathologic Features and Review of the Literature
Yoshinori Fujimotoa, Ryogo Aokib, Takuji Tanakab , Hideki Moric, d
aDepartment of Urology, Ogaki Tokushukai Hospital, Ogaki City, Japan
bDivision of Pathology, Gifu Municipal Hospital, Gifu City, Japan
cDepartment of Diagnostic Pathology, Tokushukai Hospital, Ogaki City, Japan
dCorresponding Author: Hideki Mori, Ogaki Tokushukai Hospital, Ogaki City, Gifu 503-0015, Japan
Manuscript submitted June 13, 2024, accepted August 5, 2024, published online September 16, 2024
Short title: Leiomyoma With Bladder Epithelial Dysplasia
doi: https://doi.org/10.14740/wjnu450
| Abstract | ▴Top |
Leiomyoma of the urinary bladder is a rare benign neoplasm. We report here a unique case of leiomyoma of the urinary bladder in an 82-year-old man. In the urinary bladder, transitional epithelium overlying the submucosal leiomyoma was accompanied with dysplastic changes. Morphological features of the leiomyoma and urothelial dysplasia including cytological characters are shown. Furthermore, the possible relationship between two lesions is also discussed. Present authors speculated that papillomatous nodule caused by the submucosal leiomyoma induced persistent erosive changes which led to creation of newly dysplastic cells through cellular regeneration following epithelial damage.
Keywords: Leiomyoma; Epithelial dysplasia; Urinary bladder; Cytology
| Introduction | ▴Top |
Leiomyoma is a benign circumscribed neoplasm occurring anywhere in the body. Urinary leiomyoma is a rare mesenchymal neoplasm accounting for < 1% of all bladder tumors [1, 2]. Histologically, the tumor is composed of well differentiated smooth muscle cells showing low cellularity with minimal or absent cytological atypia. As clinical features of leiomyoma of urinary bladder are rare, most tumors are detected incidentally during cystoscopy or radiological studies performed for other reasons, but some patients present with obstructive and irritative symptoms [3]. Obstructive symptoms are suggested to occur due to a ball-valve effect of a pedunculated tumor [4]. Recent reports of benign and malignant tumors of smooth muscle cells describe the current state of knowledge and the role of adjuvant therapy [5-8]. Significant trend for TP53 and RB1 mutations in leiomyosarcoma has been reported [5].
Meanwhile, urothelial dysplasia has appreciable cytological and architectural cytological features that are believed to be preneoplastic but fall short of the diagnostic threshold for urothelial carcinoma in situ [9]. Urothelial dysplasia is not well studied because it is rarely described de novo and is not typically recorded. Urothelial dysplasia harbors critical chromosome 9 deletion followed by TP53 and/or RB1 mutations [10, 11]. An interesting report on natural history of urothelial dysplasia without previous or concurrent urothelial dysplasia in situ described that significant risk for progressing to urothelial carcinoma in situ and invasive urothelial carcinoma (19% of cases with follow-up intervals ranging 6 months to 8 years) [12]. Urothelial dysplasia is often clinically silent. Patients most commonly present with symptoms relating to an associated papillary or invasive carcinoma [12].
Presently, we report an interesting case of submucosal leiomyoma associated with dysplasia of surface epithelium of the urinary bladder. Since the correlation between the subepithelial mesenchymal tumor and epithelial neoplastic changes is poorly understood, this case seems to be quite important for understanding two lesions of epithelial as well as subepithelial neoplasms.
| Case Report | ▴Top |
An 82-year-old man was referred to the Department of Urology of our hospital (Tokushukai Hospital) for a careful inspection. The patient had been notified of having microscopic hematuria in a routine health examination. He smoked 20 cigarettes/day from the age of 20 until 37 and drank beer 180 to 360 mL of sake/day. He had no constitutional symptoms except hypertension. His father died of lung cancer. Computed tomography (CT) examination of the urinary bladder displayed no clear abnormality.
In the urinary cytology, clusters of atypical urothelial deep cells with increased nuclear/cytoplasmic (N/C) ratio suggesting urothelial dysplasia (low-grade intraurothelial neoplasia) were recognized (Fig. 1). Macroscopic examination through the transurethral cystoscopy revealed a papillomatous nodule (1.0 × 1.5 cm) in the left side of the bladder. Transurethral cystoscopy with partial resection was performed. Histological examination of the resected tissue demonstrated a circumscribed lesion, which was hypocellular and was composed of bland spindle cells arranged in well-formed fascicles. The lesion was diagnosed as a leiomyoma with size of 380 µm in diameter (Fig. 2). The surface epithelium above the leiomyoma was thin. Neighboring epithelium exerted characteristics of urothelial dysplasia with loss of the perpendicular arrangement, minimal degree of nuclear enlargement and irregularity including overlapping. Umbrella cells were absent. Furthermore, there was no clear chronic inflammatory infiltrate in the mucosa (Fig. 3). Both of nuclear p53 expression and Ki-67 proliferation index in the urothelial dysplasia were > 50% (Fig. 4).
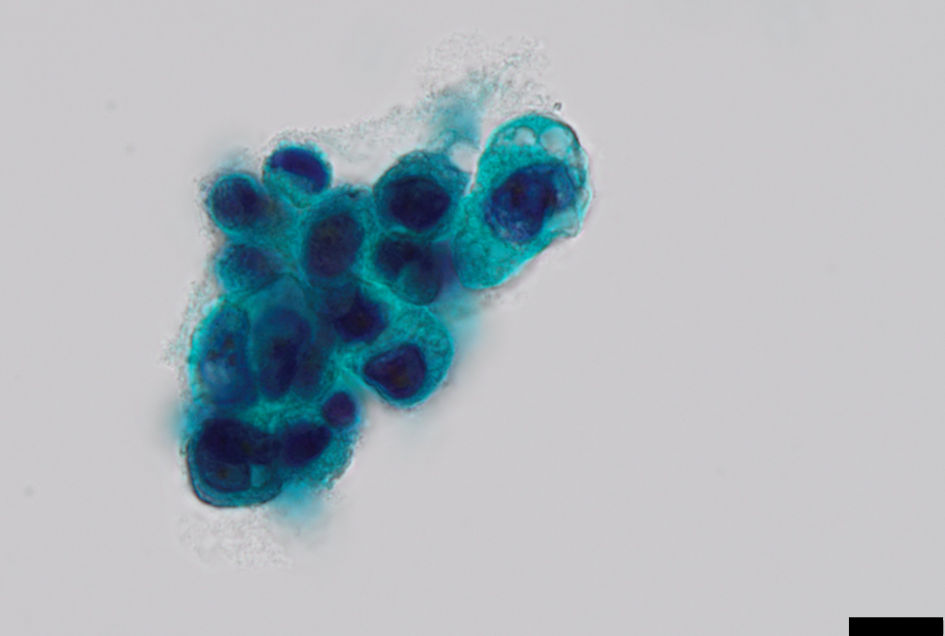 Click for large image | Figure 1. Urinary cytology showing a cluster of atypical urothelial cells with increased nuclear/cytoplastic ratio and grooved nuclei (Papanicolaou stain, scale bar = 10 µm). |
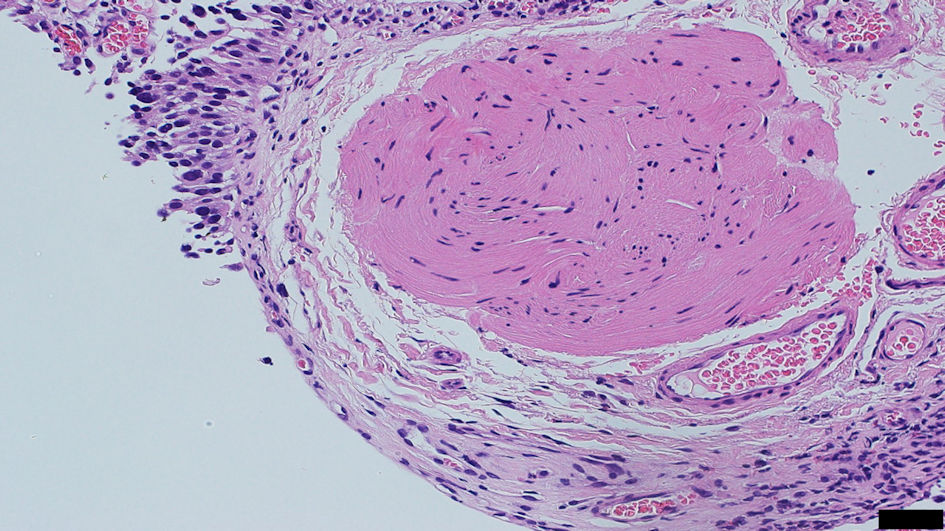 Click for large image | Figure 2. A round nodule of leiomyoma with histological features of fascicles of spindle-shaped cells with fusiform nuclei and eosinophilic cytoplasm. Overlying epithelium with erosive changes is present (hematoxylin and eosin stain, scale bar = 50 µm). |
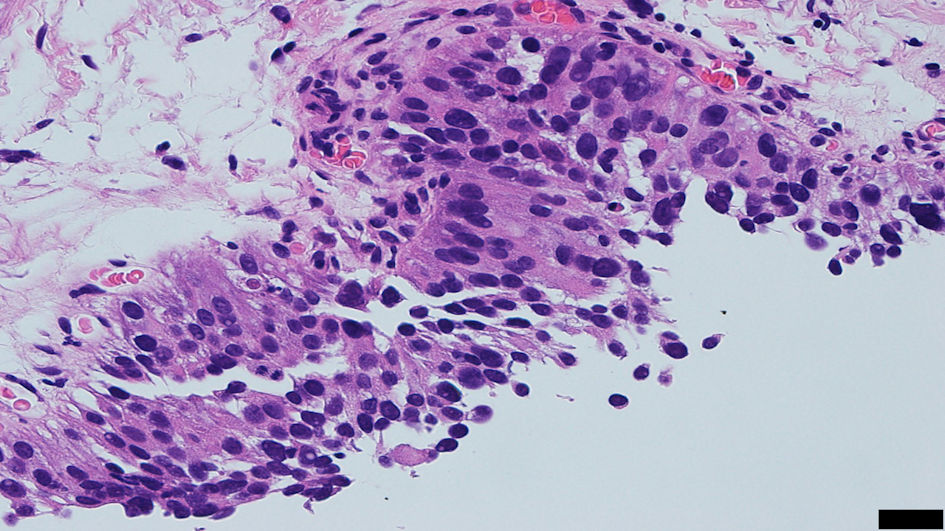 Click for large image | Figure 3. Histology of the surface epithelium with characteristics of urothelial dysplasia. The figure illustrates the loss of the perpendicular arrangement and nuclear abnormality such as enlargement, overlapping or eccentric style (hematoxylin and eosin stain, scale bar = 20 µm). |
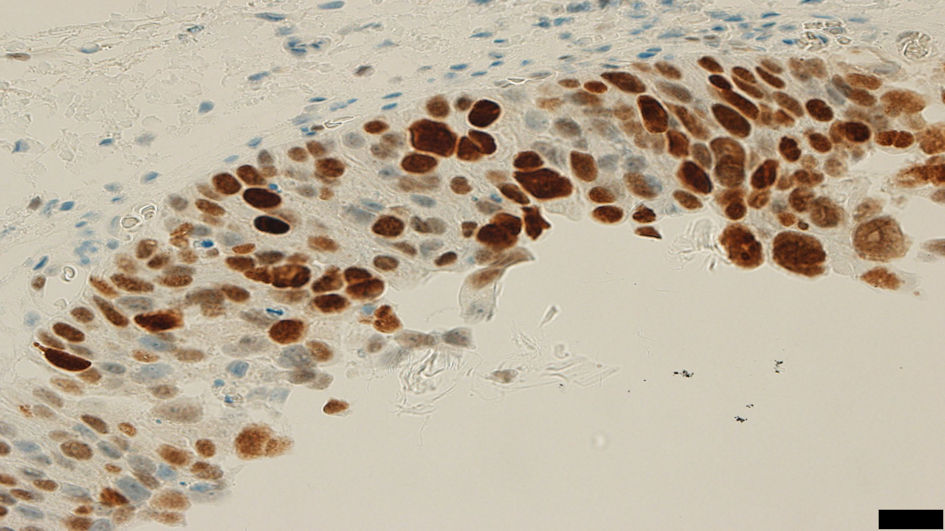 Click for large image | Figure 4. High nuclear p53 expression (> 50%) is present in the dysplastic urothelial epithelium (immunohistochemistry of p53, scale bar = 20 µm). |
| Discussion | ▴Top |
Leiomyoma is regarded as the most common benign mesenchymal neoplasm of the urinary bladder. It is also reported that the tumor has female predominance, and women making up to 76% of the patients [3]. There is also a wide patient age range at diagnosis (from 21 to 80 years) [1]. Regarding the size of the urinary leiomyoma, they tend to be 2 to 25 cm [1]. Comparing these documents, present case (82 years, male, 380 µm) may be unusual. Leiomyomas of the urinary bladder are classified into three groups based upon the location of the lesion which include 1) intravesical; 2) intramural; 3) extra-vesical leiomyoma of the urinary bladder [13]. The present case belongs to group 1. For the present case, microscopic hematuria was found occasionally. The hematuria is suggested to relate to the erosive changes of the surface epithelium. It is assumed that the submucosal leiomyoma continuously pushed up the surface epithelium, hence generated the erosions which were consistent above the neoplasm. In this case, higher values of nuclear p53 expression and Ki-67 proliferation index were present. Such evidence showing higher activity for nuclear proliferation clearly supports dysplastic nature of the surface mucosa together with the morphological properties of the epithelial overlying the myoma.
The reasons for the occurrence of epithelial dysplasia being a potent precursor lesion of urinary carcinoma are unknown. Regarding etiology of urinary bladder cancer, hereditary as well as environmental factors and other factors such as chronic inflammation have been implicated. So far as we are concerned, no reports regarding the relationship between leiomyoma and dysplasia of the surface epithelium of the urinary bladder have been documented. Certainly, the coexistence of both lesions may be coincidental. However, it may be also possible that papillomatous nodule caused by the leiomyoma induces persistent erosive changes which lead to creation of newly dysplastic cells through cellular regeneration. Ahn et al [14] described a case with epithelial lesion of severe dysplasia overlying a small leiomyoma in esophagus. Accordingly, it may be reasonable that submucosal leiomyoma has a relation to the occurrence of epithelial dysplasia.
Finally, we reported a rare case of concurrent occurrence of urothelial dysplasia and urinary bladder leiomyoma. This case suggests the gap of current state of knowledge about urothelial dysplasia and urinary bladder non-epithelial neoplasm, with a particular focus on concurrent growth of two lesions. Since both lesions may have similar gene mutations, such as TP53 and RB1 [5, 10, 11], future therapeutic strategies against these two lesions should be directed at targeting the main genetic drivers of oncogenesis.
Acknowledgments
Present authors profoundly thank Dr. Takashi Ishida, Division of Urology, Nishimino Kosei Hospital, Gifu, for providing us with important clinical information of this patient.
Financial Disclosure
None to declare.
Conflict of Interest
Authors declare no conflict of interest.
Informed Consent
Written informed consent was obtained from the patient for publication of this article.
Author Contributions
Yoshinori Fujimoto contributed to the design of the work, acquisition of data, interpretation of data, critical revision of the work for important intellectual content, final approval of the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Ryogo Aoki and Takuji Tanaka contributed to the analysis of data, interpretation of data, critical revision of the work for important intellectual content, final approval of the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Hideki Mori contributed to the conception and design of the work, analysis of data, drafting of the work, critical revision of the work, final approval of the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Cheville J, Folpe A. Mesenchymal tumours. In: Moch H, Humphrey PA, Ulbright TM, Reuter VE (editors). WHO classification of tumours of the urinary system and male genital organs. Lyon: IARC Publications; 2016. p. 126.
- Goluboff ET, O'Toole K, Sawczuk IS. Leiomyoma of bladder: report of case and review of literature. Urology. 1994;43(2):238-241.
doi pubmed - Wong FK, Wong KF, Lui CY. Urinary bladder leiomyoma. J HK Coll Radiol. 2002;5:193-196.
- Eble JN, Argani P, Grignon D, Cheng L. Tumors of the kidney, bladder, and related urinary structures. Fifth Series. In: AHornick JL (editors). AFIP atlases of tumor and non-tumor pathology. Arlington, Virginia: American Registry of Pathology; 2022. p. 504-506.
- Astolfi A, Nannini M, Indio V, Schipani A, Rizzo A, Perrone AM, De Iaco P, et al. Genomic database analysis of uterine leiomyosarcoma mutational profile. Cancers (Basel). 2020;12(8):2126.
doi pubmed pmc - Rizzo A, Nannini M, Astolfi A, Indio V, De Iaco P, Perrone AM, De Leo A, et al. Impact of chemotherapy in the adjuvant setting of early stage uterine leiomyosarcoma: a systematic review and updated meta-analysis. Cancers (Basel). 2020;12(7):1899.
doi pubmed pmc - Rizzo A, Pantaleo MA, Saponara M, Nannini M. Current status of the adjuvant therapy in uterine sarcoma: A literature review. World J Clin Cases. 2019;7(14):1753-1763.
doi pubmed pmc - Rizzo A, Ricci AD, Saponara M, A DEL, Perrone AM, P DEI, Pantaleo MA, et al. Recurrent uterine smooth-muscle tumors of uncertain malignant potential (STUMP): state of the art. Anticancer Res. 2020;40(3):1229-1238.
doi pubmed - Reuter VE, Algaba F, Amin MB, Cao D, Cheng L, Comperat E, Epstein JI, et al. Non-invasive urothelial lesions. In: Moch H, Humphley PA, Ulbright TM, Reuter VE (editors). WHO classification of tumours of the urinary system and male genital organs. IARC Publications; 2016. p. 99-107
- Inamura K. Bladder cancer: new insights into its molecular pathology. Cancers (Basel). 2018;10(4):100.
doi pubmed pmc - Musangile FY, Matsuzaki I, Iwamoto R, Sagan K, Nishikawa M, Mikasa Y, Takahashi Y, et al. Targeted next-generation sequencing of flat urothelial lesions reveals putative pathobiological pathways, potential biomarkers, and rational therapeutic targets. Mod Pathol. 2023;36(5):100120.
doi pubmed - Cheng L, Cheville JC, Neumann RM, Bostwick DG. Natural history of urothelial dysplasia of the bladder. Am J Surg Pathol. 1999;23(4):443-447.
doi pubmed - Kalathia J, Agrawal S, Chipde SS, Agrawal R. Total endoscopic management of a large bladder leiomyoma. Urol Ann. 2015;7(4):527-529.
doi pubmed pmc - Ahn SY, Jeon SW. Endoscopic resection of co-existing severe dysplasia and a small esophageal leiomyoma. World J Gastroenterol. 2013;19(1):137-140.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Nephrology and Urology is published by Elmer Press Inc.