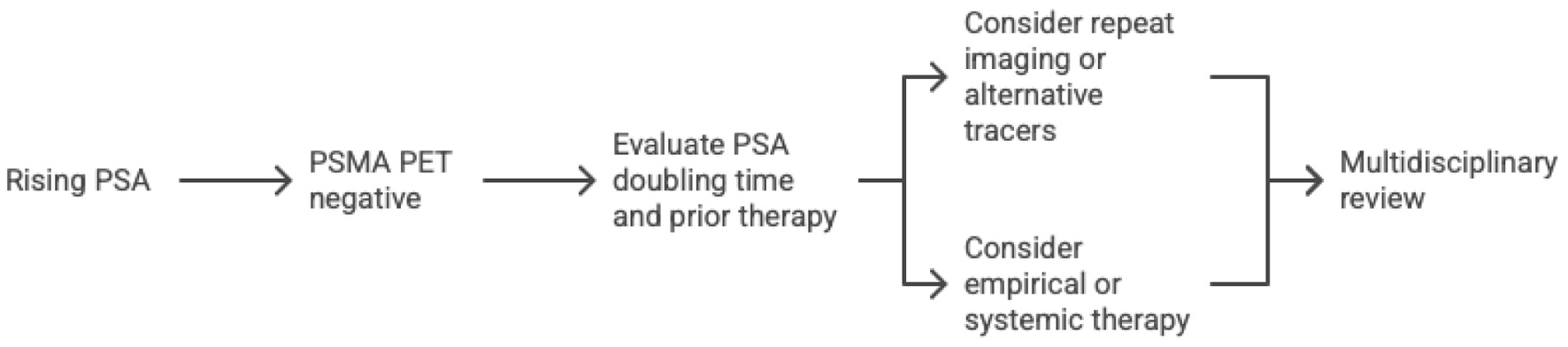
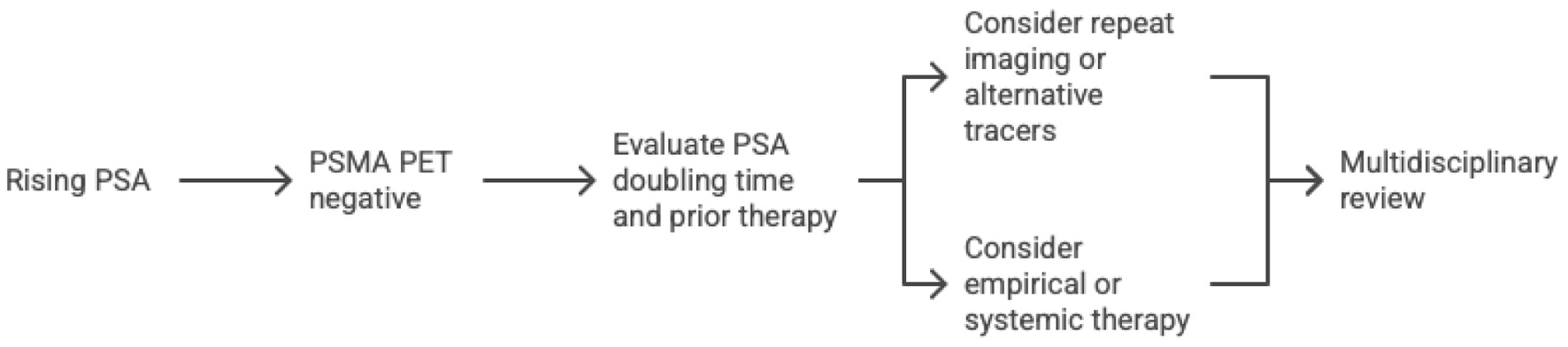
Figure 1. Proposed workflow for managing rising PSA with negative PSMA PET. PET: positron emission tomography; PSA: prostate-specific antigen; PSMA: prostate-specific membrane antigen.
| World Journal of Nephrology and Urology, ISSN 1927-1239 print, 1927-1247 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Nephrol Urol and Elmer Press Inc |
| Journal website https://wjnu.elmerpub.com |
Review
Volume 14, Number 2, November 2025, pages 27-34
Discordance Between Prostate-Specific Antigen and Positron Emission Tomography Imaging in Recurrent Prostate Cancer
Figure
Tables
| Imaging modality | Tracer/method | Typical detection sensitivity in BCR | Key limitations/considerations |
|---|---|---|---|
| This table compares common imaging options in biochemical recurrence of prostate cancer, including their typical detection sensitivity and key limitations. PET-based techniques (especially PSMA PET/CT) achieve higher detection rates at lower PSA levels compared to conventional scans [2, 9]. However, each modality has unique considerations as noted. BCR: biochemical recurrence; CT: computed tomography; MRI: magnetic resonance imaging; PET: positron emission tomography; PSA: prostate-specific antigen; PSMA: prostate-specific membrane antigen. | |||
| PSMA PET/CT (e.g., Ga-68 PSMA-11, F-18 PSMA tracers) | Radiolabeled small molecule binding PSMA on prostate cancer cells. | Highest sensitivity of available modalities. Detects ∼50% of recurrences when PSA < 0.5 ng/mL and up to ≥ 80-90% when PSA > 2 ng/mL. High specificity (∼90%); lesions as small as 2 - 5 mm may be visualized. | Limited sensitivity at very low PSA (< 0.2). False negatives occur with microscopic disease or poor PSMA expression. Uptake in benign lesions (bone islands, healing fractures, etc.) can cause false positives. Requires experienced interpretation to avoid pitfalls. Limited availability in some regions; higher cost. |
| Fluciclovine PET/CT (Axumin, F-18) | Synthetic amino acid analog taken up by cancer cells. | Moderately high sensitivity, but lower than PSMA PET at all PSA ranges. Overall detection ∼70-75%; declines to ∼20-40% when PSA < 0.5 ng/mL. Better for pelvic/local recurrences than distant in many cases. | Short tracer half-life and background muscle uptake can obscure findings. Less sensitive for small lymph nodes and distant metastases compared to PSMA. False positives from reactive lymphoid tissue possible. |
| Choline PET/CT (C-11 or F-18 choline) | Radiolabeled choline, incorporated into cell membranes. | Moderate sensitivity. Detection ∼65% overall. Works best at higher PSA; often requires PSA > 1 ng/mL for ≥ 50% detection. Poor sensitivity in early BCR (PSA < 0.5). | Very short half-life for C-11 (20 min) requires on-site cyclotron (F-18 choline has longer half-life). Lower tumor-to-background contrast than PSMA. Largely supplanted by PSMA PET in current practice due to inferior sensitivity for small lesions. |
| Conventional bone scan (99mTc-MDP scintigraphy) | Gamma camera scan detecting osteoblastic activity in bone. | Low sensitivity in biochemical recurrence unless PSA is high. Rarely detects metastases at PSA < 10 ng/mL; positive in only ∼5% of post-prostatectomy patients with PSA ∼1 ng/mL. Detection improves with PSA > 20 ng/mL. | Limited to bone metastases (cannot detect soft-tissue disease). May miss small or purely lytic lesions. False positives common (degenerative changes, arthritis can uptake tracer). Often used in conjunction with CT. Now often replaced by PSMA PET for staging and BCR imaging due to far superior sensitivity. |
| CT | X-ray-based cross-sectional imaging. | Low sensitivity for small lymph node or soft-tissue metastases. Can detect enlarged pathological lymph nodes (> 8 - 10 mm) or overt organ metastases. Often normal in BCR until disease burden is significant (e.g. bulky nodes or visceral lesions). | Limited contrast between cancerous vs normal tissue without size/structural change. Cannot reliably identify microscopic nodal metastases (a normal-sized node can harbor cancer). Often combined with functional imaging (PET) for better accuracy. Involves radiation and sometimes contrast. |
| MRI (typically multiparametric MRI for pelvis) | High-resolution anatomical imaging (with contrast and diffusion for prostate bed). | High sensitivity for local recurrence in the prostate bed or residual gland. Multiparametric MRI can detect a local tumor nodule in the prostatectomy bed at PSA levels as low as ∼0.3 - 0.5 ng/mL in some cases. Can also identify enlarged lymph nodes or bone lesions if within the field of view. | Primarily useful for local/pelvic evaluation - limited whole-body coverage (a whole-body MRI with diffusion is an emerging technique but not routine). Misses distant metastases outside scanned regions. Post-surgical or post-radiation changes can obscure or mimic recurrence. Requires expertise to interpret subtle findings. |
| PET tracer | Target mechanism | Typical detection rate | Optimal PSA range | Key comments |
|---|---|---|---|---|
| BCR: biochemical recurrence; GRPR: gastrin-releasing peptide receptor; PET: positron emission tomography; PSA: prostate-specific antigen; PSMA: prostate-specific membrane antigen. | ||||
| 68Ga-PSMA-11 | Binds PSMA transmembrane protein | 40-60% at < 0.5 ng/mL; ≥ 80% > 2 ng/mL | Any; most validated | Widely used; high accuracy |
| 18F-DCFPyL | PSMA-targeted | Similar to 68Ga-PSMA | < 0.5 ng/mL upward | Longer half-life; allows regional production |
| 18F-Fluciclovine (Axumin) | Amino-acid transport | ∼30% at 0.2 - 0.5 ng/mL | 0.5 - 5 ng/mL | Useful for local pelvic recurrence |
| 11C- or 18F-choline | Lipid membrane synthesis | 50-65% overall; poor < 1 ng/mL | > 1 ng/mL | Older agent; being replaced |
| 64Cu-SAR-bombesin/68Ga-RM2 (GRPR) | GRPR | Early data: detects 10-20% of PSMA-negative cases | PSMA-negative BCR | Under trial; complements PSMA PET |