| World Journal of Nephrology and Urology, ISSN 1927-1239 print, 1927-1247 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Nephrol Urol and Elmer Press Inc |
| Journal website https://wjnu.elmerpub.com |
Original Article
Volume 000, Number 000, January 2026, pages 000-000
Reducing Catheter Replacement Rates in Hemodialysis Patients: A Quality Improvement Initiative via Nephrologist, Surgeon, and Nursing Collaboration
Vipul Guptaa, f, Rajani Abrahamb, Rajanimol Raghunadhanb, Dalia D. Abdulrahmanc, Diary Mohammadd, Hazem Awade, Mamoun AlMarzouqid
aMohammed Bin Rashid University of Medicine and Health Sciences, Al Jalila Children Hospital, Dubai, United Arab Emirates
bDepartment of Pediatric Renal Dialysis, Al Jalila Children Hospital, Dubai, United Arab Emirates
cDubai Medical College, Dubai, United Arab Emirates
dDepartment of Pediatric Surgery, Al Jalila Children Hospital, Dubai, United Arab Emirates
eDepartment of Pediatric Nephrology, Al Jalila Children Hospital, Dubai, United Arab Emirates
fCorresponding Author: Vipul Gupta, Department of Pediatric Surgery and Urology, Al Jalila Children Hospital, Dubai, United Arab Emirates
Manuscript submitted October 28, 2025, accepted December 11, 2025, published online January 4, 2026
Short title: Reducing Catheter Replacement in HD Patients
doi: https://doi.org/10.14740/wjnu1020
| Abstract | ▴Top |
Background: Central venous catheters (CVCs) remain a common vascular access for hemodialysis (HD) initiation despite being known correlates of higher infection, hospitalization, and mortality rates. Poor coordination among dialysis nurses, nephrologists, and surgeons leads to delayed interventions for catheter dysfunction and results in unnecessary catheter replacement. The project aimed to reduce the rate of HD catheter replacement after initiation of HD below ≤ 10% through structured multidisciplinary practice.
Methods: A multidisciplinary team is developed to establish open lines of communication between nephrologists, dialysis nurses, and the surgical team so that necessary interventions can be planned in real time through monthly vascular access rounds, pre-operative huddles, urgent operating theater (OT) slots, and standardization of the catheter insertion and fixation technique.
Results: The intervention yielded noteworthy improvements in vascular access outcomes. One-year catheter survival was increased from 27% (published benchmark) to 58%, and optimal maximum catheter lifespan was extended from 158 to 376 days with average life span being 196 days. Infection rates declined from 7% to 0%. Mechanical issues including kinking reduced from 9% to 2% and catheter fracture from 4% to 0%.
Conclusion: The organization of a multidisciplinary plan substantially improved HD catheter survival and decreased complications. Improved communication and coordinated care allowed improved patient safety, decreased catheter replacement, and increased healthcare efficiency.
Keywords: Pediatric hemodialysis catheter; Quality improvement; Interdisciplinary collaboration; Catheter survival
| Introduction | ▴Top |
Vascular access is the most important determinant of effective hemodialysis (HD) and has been referred to as the “lifeline” of the patient undergoing renal replacement therapy. Despite strict guidelines for the utilization of arteriovenous fistula (AVF) or graft access, most patients, particularly children, begin with central venous catheter (CVC) access because of urgent access needs or delay in AVF maturation. CVCs do pose higher risks of infection, thrombosis, and mechanical failure and contribute to a significant portion of morbidity, hospitalization, and health care cost especially in pediatric age group [1-3]. A review of literature suggests that although adult dialysis units have been more and more embracing formal quality improvement (QI) programs and vascular access monitoring protocols, the same infrastructure in pediatric HD units worldwide is in its nascent stages. Moreover, the compromised anatomy, smaller patient size, and use of underdisciplined pediatric vascular access all make it more complex in nature especially in presence of lack of extended concerted efforts at process optimization, communication, and standardization among nephrology, surgery, and nursing specialties.
Most pediatric HD centers lack specific QI programs through which preventable complications, such as chronic catheter malfunction, infection, and premature replacement can be avoided, thus reducing procedural load on patients and healthcare systems. The financial cost of suboptimal quality systems in children undergoing dialysis is significant. Every catheter change does not only carry procedure fees, such as anesthesia, operating room, and surgical time, but also indirect hospitalization fees of antibiotics and missed dialysis sessions. Researchers have approximated that catheter infection alone adds on another 15-25% to yearly treatment fees, mostly hospitalization and extended therapy courses [4-6]. In children with limited vascular options and requiring lifetime access, planning these inefficiencies can exert significant economic and clinical consequences. Higher catheter replacement rates (42% on HD initiation) in the past at Al Jalila Children’s Hospital (AJCH) were driven mainly by delayed procedures and inconsistent communication between dialysis nurses, surgeons, and nephrologists. Common care barriers included imprecise referral roles, inadequate urgent operating room time, and inconsistent catheter care practices. Upon realizing the importance of an optimized, team-oriented effort, a multidisciplinary group conceptualized and launched a QI initiative to drive optimal collaboration among the three main stakeholders, nephrologists, surgeons, and nurses, toward improving vascular access survival, patient safety, and healthcare efficiency. This project therefore had the double benefit of reducing catheter replacement rates and demonstrating how the application of structured QI principles to pediatric dialysis can create measurable improvements in clinical outcomes, cost-effectiveness, and interprofessional coordination.
| Methods | ▴Top |
The primary objective of the present QI project was to reduce the frequency of catheter replacements following HD initiation to ≤ 10% in 6 months using formal interprofessional communication and standardized care pathways. The project was implemented at the AJCH Dialysis Unit between January and December 2024 based on the principle of plan-do-study-act (PDSA) model (Table 1) and the outcome was compared with benchmark data reported in literature and experienced in pediatric nephrology unit from January 2023 till December 2023. A multidisciplinary team was brought together consisting of nephrologists, surgeon, and dialysis nurses who collaborated closely with each other in all PDSA cycles.
 Click to view | Table 1. Results and Outcome of QI Project FOCUS-PDSA |
Interventions were directed at three main areas: communication and coordination, standardization of procedures, and catheter maintenance and care. Regular multidisciplinary vascular access rounds were conducted once a month to promote communication and coordination and allow direct interaction between dialysis nurses, nephrologist, and surgeon. Emergency referral channels were also put in place to allow for prompt assessment and intervention for catheter failure, thereby reducing delays in decision-making and procedural planning. Procedural standardization was achieved by pre-procedure huddles between dialysis and surgical teams to determine the corresponding catheter size and location for a patient. A dedicated urgent operating theater (OT) slot was kept for access procedure-related surgeries to minimize waiting times. Dedicated morning rounds by the surgical team was performed once procedures were done to enable early detection of catheter complications and hence prevention of complications in subsequent cases.
Standardized catheter care and maintenance procedures were adopted across the unit. A uniform fixation practice was used by the team with substitution of Prolene sutures by Mersilk, which improved catheter stability and minimized mechanical irritation. Sutures and skin glue over the exit site were not applied to prevent granuloma and site cleanliness misinterpretation. Nurses received education on new dressing procedures to ensure standardized and aseptic vascular access care.
Data were obtained prospectively from patient charts and dialysis unit logbooks. The parameters like insertions, replacements, survival duration, infection, and mechanical complications were quantified.
Pre- and post-intervention data and baseline data, as well as published standards, were compared. Real-time feedback and data analysis within each PDSA cycle initiated iterative change. Communication breakdown was recognized in the first cycle and necessitated the formation of a nurse-nephrologist-surgeon communication group and emergency referral line. The second cycle touched on surgical backlog of schedules by introducing a fixed urgent OT slot. The third cycle touched on fewer infections by modifying fixation materials and removal of skin glue, and the fourth cycle enhanced usual multidisciplinary review meetings and inclusion of the project in the hospital QI audit calendar with a trial to sustain enhanced outcomes (Fig. 1).
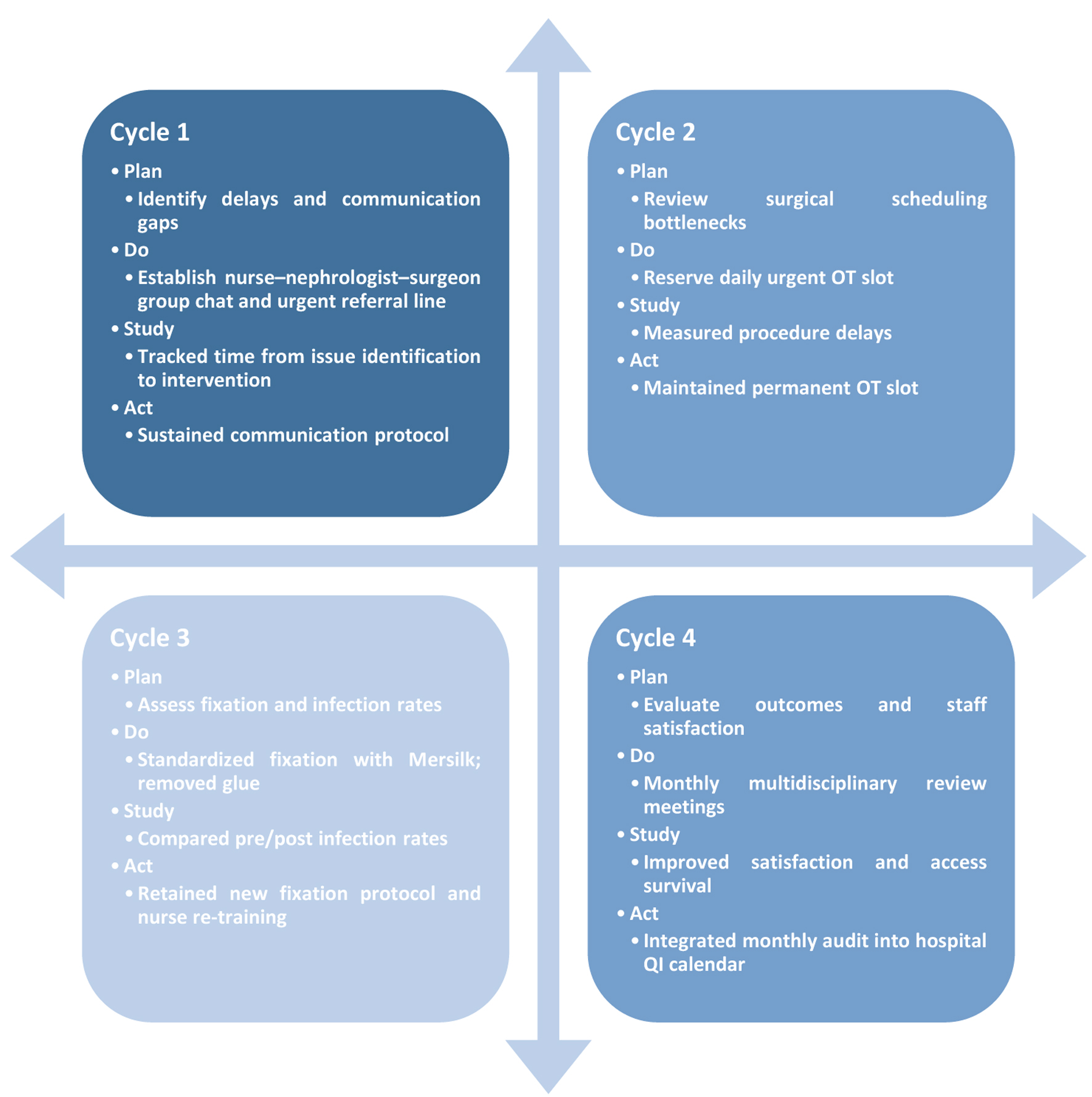 Click for large image | Figure 1. Plan-do-study-act approach. |
| Results | ▴Top |
Following the introduction of QI interventions, a total of 21 patients underwent HD catheter insertion and the outcome was compared with 22 cases who underwent HD catheter insertion from January 2023 till December 2023. The project achieved substantial improvements in catheter survival, complication rate, and overall vascular access outcomes. One-year catheter survival was enhanced from a reported baseline of 27% to 58% at AJCH, representing a 115% increment. In a similar fashion, optimal maximum catheter length improved from 158 to 376 days in seven patients, representing a 138% improvement in length.
Complication rates decreased profoundly in all parameters being monitored. Infection rate was reduced from 7% to 0%, completely eliminating catheter-related infections during the study period. Even mechanical complications improved significantly: kinking of catheters was reduced from 9% to 2%, a reduction of 78% mainly owing to standardization of insertion technique and implementation of standardized catheter care skills in form of proper handling of hub, positioning of patient and regular monitoring of catheter for any twist or improper clamp placement. The incidence of catheter fracture reduced from 4% to 0% owing to use of Mersilk suture for securing wings which provided less shearing effect on delicate pediatric skin as compared to Prolene suture in pre-intervention period, thus providing stability to catheter for longer period. Presence of glue at exit site in pre-QI cohort often results in accumulation of dust thus deceiving nursing staff for presence of infection. This results in formation of granuloma and often repeated attempts to clean it, not only causing discomfort to pediatric patients but resulting in accidental pulling of catheter at time of first dressing change in one case where glue was adherent to dressing.
Composite replacement rate for catheters overall diminished from baseline 42% to 12%, near goal of ≤ 10%. The main reason of catheter replacement before implementation of project appeared to be poor flow rates and exteriorization of cuff. A lack of communication usually resulted in insertion of improper size of catheter in one patient and tight sutures at exit site in two patients, making it difficult to achieve target flow rates. After implementation of project, none of patients required catheter replacement due to poor flow rates which largely resulted from improved communication across disciplines, uniform procedural planning, and proactive management of complications related to access (Fig. 2). Six patients had exteriorization of cuff on pre-QI cohort which required replacement of catheter which was attributed to presence of Prolene as fixation stich. Prolene sutures being monofilament often appeared to come out early owing to delicate pediatric skin especially in uremic patients where the weight of catheter flange often results in shearing forces and dislodgement of catheter before cuff is fixed.
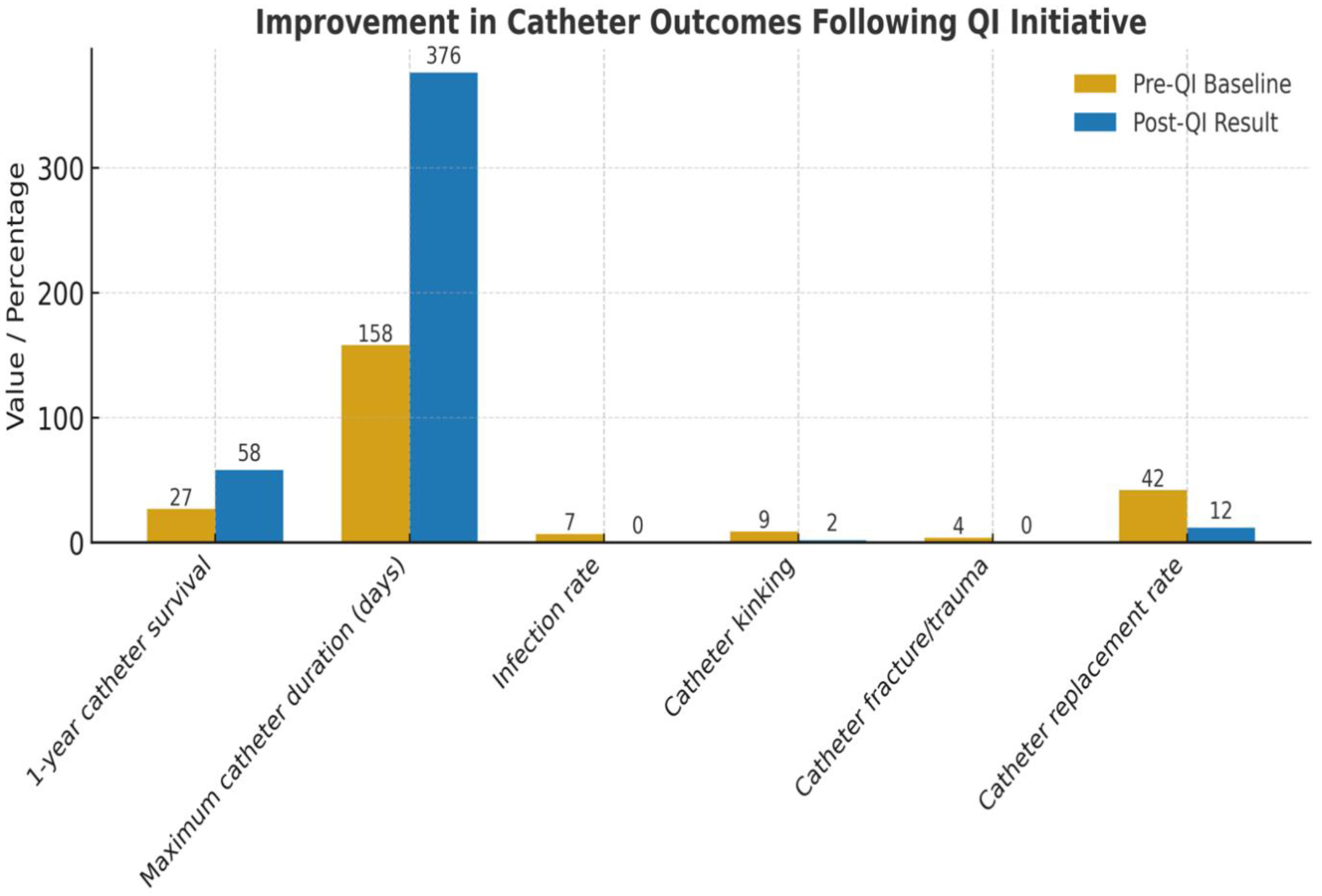 Click for large image | Figure 2. Chart showing pre- and post-QI project results. QI: quality improvement. |
Comparison with pre-QI and benchmark data (Table 1) disclosed that composite outcomes of enhanced coordination, procedural consistency, and maintenance practices showed clear and lasting improvement in patient safety, resource utilization, and vascular access durability.
| Discussion | ▴Top |
This QI project demonstrated that coordinated interdisciplinary collaboration was able to dramatically enhance HD vascular access outcomes. By uniting nephrologists, surgeons, and dialysis nurses under a single system of communications, our organization was able to achieve marked improvements in catheter survival, eliminate catheter-related infections, and minimize mechanical complications. The success so observed speaks to the basic premise that vascular access management is not the interest of a single specialty but a shared clinical responsibility with spontaneous coordination and consistent practices. The characteristic of the project was the institutionalization of collaboration among the three principal stakeholders, nephrologists, surgeons, and dialysis nurses, each having a different yet complementary role. Prior to the intervention, disorganized communication frequently delayed decision-making, resulting in prolonged catheter dysfunction, additional replacements, and risk of infection. Being provided with a direct referral pathway and monthly review meetings for vascular access provided scope for shared decision-making and the early identification of malfunctioning catheters.
This model best complies with the principles advocated by the Kidney Disease Outcomes Quality Initiative (KDOQI) and all ensuing international guidelines for vascular access, supporting the “Vascular Access Team” model. It has been consistently demonstrated in research time and again that centers with operative multidisciplinary access teams have reduced catheter-related bloodstream infections (CRBSI), improved fistula maturation, and fewer urgent procedures [1-3]. Our findings support this paradigm by demonstrating measurable gains in outcomes when communication barriers are systematically overcome. A 0% rate of infection during the trial period is a superior outcome that demonstrates the effectiveness of standardizing catheter insertion and care protocols. The literature indicates that catheter-related infections are a major cause of morbidity and mortality in pediatric HD patients, accounting for nearly one-third of hospitalizations due to access [4, 5].
Our infection-free results likely are the result of two interventions: 1) improved fixation and exit-site care, and 2) enhanced staff knowledge through education and feedback loops. The Prolene to Mersilk suture change reduced mechanical irritation and exit-site trauma, and discontinuation of skin glue prevented debris accumulation and misreading dressing cleanliness. Standardization has been demonstrated to reduce variation, a phenomenon QI science embraces and previously has been demonstrated to reduce CRBSI rates to near zero in highly coordinated systems [6]. The present pediatric nephrology center has well established renal transplant program. Most of parents do not prefer AVF and usually undergo renal transplant early, hence AVF is not practiced in this center.
The dramatic reduction in mechanical issues, including kinking and fracture, suggests that preoperative huddles between surgeons and dialysis personnel contribute significantly to long-term catheter success through careful planning regarding site, size, and dressing. This is further supported by the presence of adversarial reports indicating that mallocation or inappropriate catheter size causes malfunction and unnecessary replacement [7, 8]. Individualized selection of access by collective discussion allowed our unit to extend the longest catheter survival time from 158 to 376 days, more than a doubling of functional duration. Such a gain not only suggests increased technical precision but also improved post-operative follow-up and nursing care. Daily dialysis rounds with continual presence of the operating team permitted immediate feedback and intervention when initial warning signs of dysfunction were apparent.
Systematically, using the QI methodology in the form of the PDSA model, it was possible to pilot process changes step by step and then continuously track them. All intervention cycles were evidence-based and guided by real-time feedback from the multidisciplinary team. The ensuing efficiency gains were multipronged: reduced use of emergency OT, since fewer emergency replacements meant optimized operating room planning and utilization; increased nurse participation through structured communication that enabled nursing staff to bring up access issues early and in a timely manner and confidently; and maximized patient safety by enabling early treatment prior to clinical deterioration. These synergistic improvements underscore the importance of embedding QI frameworks in routine clinical governance in dialysis units. This is in line with other United States and United Kingdom initiatives that have reported corresponding decreases, where catheter complication rates fell by 40-60% following the adoption of team-based QI models [9, 10].
Reducing frequency of replacement of catheters translates proportionally to decreased hospitalization and procedural treatment, lowering healthcare system cost and burdens. Each replacement of a catheter not only carries procedure-associated risk but also includes indirect costs of anesthesia, infection control, and potential central venous stenosis. In addition, improved catheter survival benefits the patient by minimizing procedure-associated anxiety and interruption of dialysis schedules, an effect directly correlated with treatment compliance and quality of life. In children, where vascular access options are limited, optimizing catheter survival is of even more clinical importance.
Our findings are consistent with published international experience. Whereas global reports cite 4-10% rates of annual CVC infection and mean catheter survival of 100 - 200 days, our project recorded a 0% infection rate and average catheter longevity of well over 196 days. These outcomes place the AJCH Dialysis Unit among world-leading performing centers and affirm the effectiveness of site-specific QI translation in the UAE healthcare context. The magnitude of our improvement is equaled by research by Toma et al (2019) and Albalate et al (2020), both of which indicated that team-oriented, organized interventions are one of the best predictors of the success of vascular access.
Despite the very promising results of this QI project, there are a few limitations to be mentioned. The research was conducted in a single large tertiary pediatric hospital with a similarly modest patient volume, which will limit generalizability to some degree. In addition, while process compliance was monitored, formal statistical comparison of pre- and post-intervention data could not be undertaken due to small sample size. Future studies should incorporate multicenter participation, larger patient datasets, and extended monitoring for more than 1 year to assess long-term durability. Additionally, addition of patient and caregiver feedback could offer a valuable addition to subsequent quality measures.
In conclusion, this QI project demonstrates how long-term interdisciplinary collaboration, process standardization, and preventive communication can transform vascular access outcomes (Fig. 3). The intervention not only improved catheter survival and eliminated infection but also enhanced staff coordination and process optimization. These findings provide a usable blueprint for dialysis units interested in improving vascular access care and patient safety through effective, team-based quality improvement.
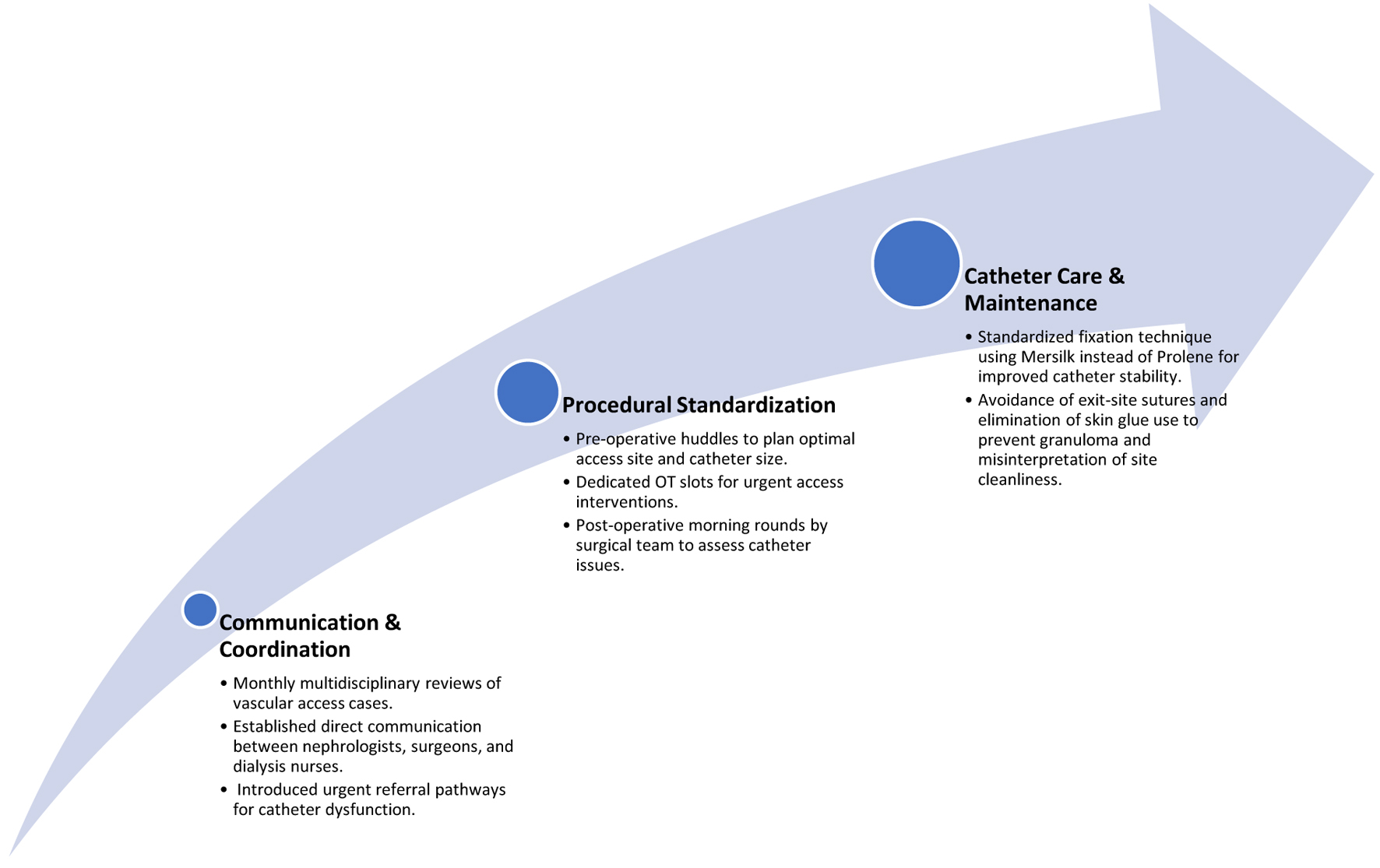 Click for large image | Figure 3. Focus pathway of QI project. QI: quality improvement. |
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
VG: data retrieval, analysis, and manuscript draft and submission; RA and RR: data retrieval, analysis, literature review, and feedback; DDD: literature review; DM: data analysis and manuscript review; HA: data retrieval, analysis, and manuscript draft and feedback; MM: data analysis, manuscript review, and feedback.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Allon M, Brouwer-Maier DJ, Abreo K, et al. Complications of hemodialysis catheters: beyond infection. Clin J Am Soc Nephrol. 2019;14(7):1017-1026.
- Moist LM, Lok CE. Vascular access: the Achilles’ heel of hemodialysis. Clin J Am Soc Nephrol. 2020;15(10):1491-1493.
- Chand DH, Valentini RP, Kamil ES. Hemodialysis vascular access in children: challenges and outcomes. Pediatr Nephrol. 2020;35(5):829-840
- Lee T. Fistula first initiative: historical impact and future directions. Semin Dial. 2021;34(4):259-265.
- Harish A, Allon M. Communication gaps and missed opportunities in vascular access care. Am J Kidney Dis. 2020;76(1):143-151.
- Lok CE, Huber TS, Lee T, Shenoy S, Yevzlin AS, Abreo K, Allon M, et al. KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. Am J Kidney Dis. 2020;75(4 Suppl 2):S1-S164.
doi pubmed - Albalate M, Perez-Garcia R. Preventing catheter-related bloodstream infections in hemodialysis: lessons from successful programs. Nefrologia. 2020;40(6):599-607.
- Taylor G, Gravel D, Johnston L, et al. Prospective surveillance for primary bloodstream infections in hemodialysis patients. Am J Infect Control. 2020;48(12):1552-1559.
- Toma S, Shingarev R, Allon M. Interdisciplinary approach to reduce hemodialysis catheter malfunction. J Vasc Access. 2019;20(2):156-163.
- Wang W, Kliger AS, Ginsberg N. Cost-effectiveness of vascular access quality improvement programs. Kidney Int Rep. 2021;6(3):587-559
This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY 4.0), which permits unrestricted use, distribution, and reproduction in any medium, including commercial use, provided the original work is properly cited.
World Journal of Nephrology and Urology is published by Elmer Press Inc.